By Gretchen Green, MD, MMS
What is an ectopic pregnancy?
An ectopic pregnancy is a pregnancy that develops in an abnormal location outside or within the uterus (womb). The incidence of ectopic pregnancy has been increasing over time, to a current estimate as high as 2% of all pregnancies.(1) Patients with a history of infertility treatment or prior ectopic pregnancy are at higher risk than the average woman.(2) Women with ectopic pregnancy risk bleeding and potential death due to hemorrhage (blood loss) if the abnormal pregnancy grows too large and tears surrounding tissue (rupture). Therefore, the goal is to diagnose ectopic pregnancy as early as possible, and with the greatest degree of accuracy.
How is ectopic pregnancy diagnosed?
Before the routine use of imaging exams such as ultrasound, ectopic pregnancy was diagnosed clinically and often only after rupture, necessitating emergency surgery and often with high mortality. Ultrasound can now be used to diagnose an intrauterine pregnancy as early as approximately 5 weeks gestational age, before a woman may even realize she is pregnant.
How can ultrasound diagnose ectopic pregnancy?
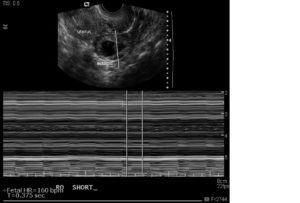
Ultrasound is a medical test using sound waves to image tissue noninvasively. The lack of radiation makes it popular in obstetrics to reduce the risk of exposure to both mother and fetus. As ultrasound resolution has improved, ultrasound has become better able to diagnose the different stages of early pregnancy, especially with transvaginal probes that are inserted into the vagina and provide a close-up view of the uterus and ovaries. A confident diagnosis of ectopic pregnancy can be made when a gestational sac, yolk sac, and fetal pole with cardiac activity are seen outside the normal location within the uterus, as in the ectopic pregnancy shown in Figure 1.
Figure 1. Ultrasound image of right-sided ectopic pregnancy outside the uterus (labeled). The fetal pole (embryo) with cardiac activity (vertical lines indicating heart rate measurement in beats per minute) is visible.
Visualization of a normal intrauterine pregnancy makes the diagnosis of ectopic pregnancy unlikely; ectopic pregnancy can coexist with an intrauterine pregnancy (termed heterotopic pregnancy) but this is rare.(3) However, the converse is not necessarily true; if neither an intrauterine nor ectopic pregnancy is seen at ultrasound, the risks and benefits of treatment for presumptive ectopic pregnancy should be considered before using medical treatment such as methotrexate.(4) The development of both normal pregnancies and ectopic pregnancy proceeds along a spectrum of findings at ultrasound, and diagnosis may not always be definitive based on the findings seen at the time of the exam.
What are the potential risks of litigation regarding ultrasound and ectopic pregnancies?
If no intrauterine pregnancy is seen in a woman with a positive pregnancy test, diagnostic possibilities include normal intrauterine pregnancy too early to be seen, ectopic pregnancy, and miscarriage. (Figure 2)
Figure 2: No intrauterine pregnancy is visible in this patient; the location of the pregnancy is unknown. A surgically proven left-sided tubal ectopic pregnancy was later diagnosed.
If a woman is presumptively diagnosed with an ectopic pregnancy and given methotrexate, and is later found to have an intrauterine pregnancy instead, there is a risk of birth defects or miscarriage as side effects of methotrexate.
If a blood test called quantitative β-hCG is used to attempt to increase the sensitivity of diagnosis of ectopic pregnancy, correlation with ultrasound findings may help reduce the risk of misdiagnosis and potential harm to an intrauterine pregnancy.
Physicians interpreting ultrasound should be familiar with the development of normal and ectopic pregnancies as well as potential pitfalls in diagnosis.
Litigation may result from either failing to diagnose an ectopic pregnancy or treating a pregnancy as ectopic when it in fact was not ectopic. An obstetrical ultrasound expert witness may be called in such cases to opine on the standard of care and whether or not that standard was breached regarding the ectopic pregnancy imaging. Additionally, expert witnesses on β-hCG and methotrexate may also be called. The β-hCG and methotrexate expert witness may discuss whether treatments were appropriate and whether any treatment resulted in harm to the fetus (causation expert witness).
Conclusion
An expert witness knowledgeable about the topic of ultrasound diagnosis of ectopic pregnancy may be a valuable resource to attorneys encountering cases of alleged missed diagnosis of ectopic pregnancy.
About the author:

Dr. Green has lectured nationally on diagnostic radiology topics and co-authored two breast imaging textbooks with colleagues at Harvard’s Brigham and Women’s Hospital. She has been retained in multiple cases as an expert witness in obstetrical ultrasound, breast imaging, body imaging (CT, MRI, and ultrasound), and general radiology. Dr. Green has served as a clinical medical director of both mammography and ultrasound for a large private practice and a reviewer of educational exhibits for publication in Radiographics, the educational journal for the Radiological Society of North America.
Contact Dr. Green at:
336 501 3151 (cell)
References
- Kao LY, Scheinfeld MH, Chernyak V, Rozenblit AM, Oh S, Dym RJ. Beyond ultrasound: CT and MRI of ectopic pregnancy. AJR American journal of roentgenology. 2014;202(4):904-11.
- Levine D. Ectopic pregnancy. Radiology. 2007;245(2):385-97.
- Dibble EH, Lourenco AP. Imaging Unusual Pregnancy Implantations: Rare Ectopic Pregnancies and More. AJR American journal of roentgenology. 2016;207(6):1380-92.
- Doubilet PM, Benson CB. First, do no harm… To early pregnancies. Journal of ultrasound in medicine: official journal of the American Institute of Ultrasound in Medicine. 2010;29(5):685-9.