By Gretchen Green, MD, MMS
Introduction
An alleged delayed diagnosis of lung cancer can result in a medical malpractice claim. In such claims, the issue of when a radiologist is under a duty to call the referring physician may come up. In such cases, a pulmonary nodules radiology expert witness may be utilized by counsel.
How are pulmonary nodules detected?
Radiologists (physicians who read imaging exams including chest radiographs and CT) typically diagnose pulmonary nodules on imaging performed to evaluate respiratory symptoms or unrelated medical problems. Pulmonary nodules may not be visible on radiographs if < 1 centimeter in diameter, but may be seen when as small as several millimeters on newer CT scans with thin image slices. The risk of lung cancer in a 6mm nodule is approximately 1%, which has been selected as a threshold necessitating follow up imaging or workup according to the 2017 Fleischner Society guidelines.[1] Other imaging features including spiculation (irregular edges), upper lobe position, and smoking history may increase the chances of lung cancer. Detecting lung cancer early may improve a patient’s chances of survival, but not all lung nodules will turn out to be cancerous.
Figure 1: Transverse 1-mm CT section through the left upper lobe shows a suspicious solid spiculated nodule (arrow). Surgery revealed invasive adenocarcinoma. (Source: Reference 1 (MacMahon et al 2017, available via free access online at https://pubs.rsna.org/doi/10.1148/radiol.2017161659).
How are pulmonary nodules evaluated?
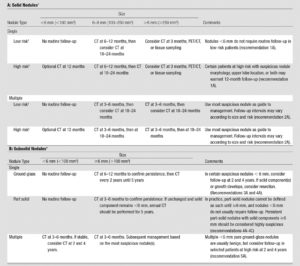
As improved imaging technology has enabled better visualization of pulmonary nodules, the Fleischner Society provided guidance for reporting and follow up imaging in multidisciplinary guidelines initially published in 2005.[2]
With continued improvements in imaging and the emergence of results from longitudinal follow-up patient clinical trials, subsequent Fleischner Society criteria revisions addressed the need for follow up of smaller nodules and those with newly-seen features such as different internal shades of grey (ground-glass nodules).[3] These criteria attempt to balance the potential harms of radiation from follow-up imaging exams or biopsies with the risk of death from lung cancer.
Figure 2: Fleischner Society 2017 Guidelines for Management of Incidentally Detected Pulmonary Nodules in Adults (Source: Reference 1 (MacMahon et al 2017, available via free access online at https://pubs.rsna.org/doi/10.1148/radiol.2017161659)
Radiology Standard of Care Issues Regarding Pulmonary Nodules
Radiologists typically dictate findings into reports that are now commonly transmitted electronically to referring clinicians. Nonroutine communication methods including a direct phone call to the clinician or even the patient may be indicated if a finding could potentially cause harm if not acted upon. The American College of Radiology Practice Parameter for Communication of Diagnostic Imaging Findings Revised 2014 provides guidance for communication but does not specifically mandate that all pulmonary nodules be specifically called to the referring clinician. [4]
Dr. Leonard Berlin has opined that radiologists should call referring clinicians if a pulmonary nodule is large enough to need imaging follow up according to the Fleischner Society criteria.[5] However, Dr. Berlin also acknowledges that this is not mandatory, and that there is some risk involved in both calling or not calling referring clinicians. Distractions from constant phone calls can lead to medical errors, as can a potentially lost report with significant imaging findings.
Physicians interpreting chest radiographs and CT should be familiar with the appearance and management of pulmonary nodules.
Litigation may result from failing to recognize or report a potentially significant pulmonary nodule, recommend appropriate follow up or additional testing, or a disruption in the chain of communication in reporting this finding. A radiology expert witness may be called in such cases to opine on the standard of care and whether or not that standard was breached regarding the pulmonary nodule imaging or follow-up.
Conclusion
A pulmonary nodules radiology expert witness may be a valuable resource to attorneys encountering cases of alleged missed diagnosis of lung cancer. Such a lung cancer expert witness may be asked to address the issues of standard of care and breach in a medical malpractice case.
About the author:
Gretchen Green, MD, MMS is a diagnostic radiologist in active clinical practice since 2006. She completed a fellowship at Harvard’s Brigham and Women’s Hospital including reading specialty chest CT and chest radiographs after completing a diagnostic radiology residency at Yale. She earned an undergraduate Sc.B. degree in neuroscience, a masters in medical science degree in the history of medicine and pharmacology, and a medical degree with academic honors, all from Brown University.
Dr. Green has lectured nationally on diagnostic radiology topics and co-authored two breast imaging textbooks with colleagues at Harvard’s Brigham and Women’s Hospital. She has been retained in multiple cases as an expert witness in chest radiology, obstetrical ultrasound, breast imaging, body imaging (CT, MRI, and ultrasound), and general radiology. Dr. Green has served as a clinical medical director of both mammography and ultrasound for a large private practice and a reviewer of educational exhibits for publication in Radiographics, the educational journal for the Radiological Society of North America.
Contact Dr. Green at: 336 501 3151 (cell), drgreen@gretchengreenmd.com
[1] MacMahon, H., et al. (2017). “Guidelines for Management of Incidental Pulmonary Nodules Detected on CT Images: From the Fleischner Society 2017.” Radiology 284(1): 228-243.
[2] MacMahon, H., et al. (2005). “Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society.” Radiology 237(2): 395-400.
[3] Naidich, D. P., et al. (2013). “Recommendations for the Management of Subsolid Pulmonary Nodules Detected at CT: A Statement from the Fleischner Society.” Radiology 266(1): 304-317.
[4] ACR Practice Parameter for Communication of Diagnostic Imaging Findings Revised 2014, accessed online 4/1/20. Available at https://www.acr.org/-/media/ACR/Files/Practice-Parameters/CommunicationDiag.pdf?la=en
[5] Berlin, L. (2018). “Medicolegal-Malpractice and Ethical Issues in Radiology: Should I Call the Referring Physician for Every Lung Nodule I See?” AJR Am J Roentgenol 211(2): W132.