Introduction
Persistent pulmonary hypertension in the newborn (PPHN) occurs when after the baby is born the blood vessels in the lungs do not open up enough and not enough blood gets into the lungs to pick up enough oxygen for the baby. The baby remains blue and the amount of oxygen getting to the brain and other organs is reduced. This is why PPHN is so dangerous. Babies born with PPHN are at high risk for neurodevelopmental impairments, hearing loss, and death. In many cases, neonatal expert witnesses are called upon to evaluate whether the standard of care was met before, during, and after delivery.
When PPHN arises in obstetric medical malpractice cases, it is usually allegations of failure on the part of doctors or hospital staff to administer immediate and proper respiratory assistance after birth. Doctors must promptly diagnose PPHN and be fully prepared to engage in emergency neonatal resuscitation procedures.
Lack of Oxygen
During pregnancy, the baby gets its oxygen from its mother through the placenta. Very little blood goes to the baby’s lungs because the blood vessels in the baby’s lungs are mostly closed. Following a normal pregnancy and a normal delivery, a baby starts taking his or her first breaths of air and the blood vessels open up. This allows the blood to travel from the baby’s heart through small blood vessels lining the air sacs in the lungs where the blood picks up oxygen. The baby turns pink and he/she starts breathing normally within minutes after birth, without any distress and getting enough oxygen for the brain and the rest of the body.
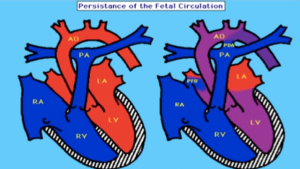
PPHN happens when after the baby is born, the blood vessels in the lungs do not open up enough and not enough blood gets into the lungs to pick up enough oxygen for the baby. This is illustrated in the picture below:
On the left the “blue” blood is pumped by the right ventricle (RV) through the pulmonary artery (PA) into the lungs. The “blue” blood gets “pink” as it travels through the lungs and picks up oxygen from the air sacs of the lungs and the “pink” blood is pumped out to the brain and the rest of the body by the left ventricle (LV) through the aorta (AO).
The picture on the right shows the flow of blood that occurs in babies with PPHN. In PPHN, the lung’s blood vessels do not allow blood to enter the lungs easily and the “blue” blood bypasses the lungs and enters the aorta through the patent ductus arteriosus (PDA).
Depending on how severely the blood vessels in the lungs are closed down, the more “blue” the baby will be and in grave danger of not getting enough oxygen.
Causes of Persistent Pulmonary Hypertension of the Newborn.
PPHN is a very uncommon condition, occurring in about 0.4 to 6.4 babies per 1000 live births.
Some of the potential causes of PPHN include:
- Post-term deliveries or during full-term, stressful births
- Maternal infections that are passed on to the fetus
- Birth Asphyxia (decreased oxygen being transferred to the baby around the time of birth)
- Abnormal lung growth or underdeveloped lungs
- Mother’s use of certain antidepressant medications during pregnancy: primarily selective serotonin reuptake inhibitors (SSRI’s) such as Paxil, Zoloft, and Prozac
- Neonatal Respiratory Distress Syndrome
- Meconium Aspiration Syndrome
- Fetal Distress (abnormal fetal heart tracings indicative of fetal distress and lack of adequate oxygen transfer through the placenta)
Symptoms and Signs Associated with PPHN.
The vast majority of cases involving Persistent Pulmonary Hypertension of the Newborn will present symptoms immediately after birth or within the first 12 hours after delivery.
- Labored breathing (respiratory distress)
- Rapid breathing (tachypnea)
- Rapid heart rate (tachycardia)
- Blue-tinted lips and/or skin (cyanosis)
- Low levels of oxygen in the blood (hypoxia)
- Looks sick at birth or in the first hours after birth (neonatal distress)
PPHN is often associated with the following signs and symptoms of perinatal distress:
- Low Apgar Scores, need for resuscitation and oxygen at the time of birth, meconium staining of amniotic fluid
It is absolutely essential that doctors and medical professionals identify the babies who are at risk to develop PPHN and initiate therapies to prevent the development of PPHN.
Diagnosis of PPHN
This diagnosis is usually made within the first few hours of life, usually within 12 hours.
Laboratory Testing
- Arterial blood gas levels. It is very important that an arterial blood PaO2 is measured as oxygen saturation measurements can be misleading. Oxygen saturation may be high in the 90-95% range even when PaO2 is low because of the high fetal hemoglobin present in newborn babies.
- Complete blood cell count with differential: high hematocrit level can exacerbate PPHN. Rule out infection.
- Coagulation studies
- Serum electrolytes
Imaging Studies
- Chest Radiography: To assess for presence of underlying lung disease (e.g., meconium aspiration syndrome, pneumonia, surfactant deficiency)
- Echocardiography This is considered the most reliable noninvasive test to establish the diagnosis, assess cardiac function, and exclude associated structural heart disease.
- Cranial Ultrasonography: To assess for intraventricular bleeding and for peripheral areas of hemorrhage or infarct if ECMO is being considered
- Cardiac Catheterization: Rarely utilized to exclude congenital heart disease (e.g., obstructed anomalous pulmonary venous return, pulmonary vein stenosis) because echocardiographic findings are typically diagnostic.
Treatment of PPHN
The goal of treatment for PPHN is to increase the delivery of oxygen to all of the baby’s body.
General Management
- Continuous monitoring of oxygenation, blood pressure, and perfusion
- Maintaining a normal body temperature
- Correction of electrolytes/glucose abnormalities and metabolic acidosis
- Nutritional support
- Minimal stimulation/handling of the newborn
- Minimal use of invasive procedures (e.g., suctioning)
Medical Therapy
PPHN treatment may consist of the following:
- Drugs to improve systemic blood pressure
- Surfactant administration: For premature and full-term newborns with surfactant deficiency
- Endotracheal intubation and mechanical ventilation: high-frequency ventilation
Pharmacotherapy
- Inhaled nitric oxide
- Other drugs such as phosphodiesterase inhibitors, endothelin receptor antagonists
Extracorporeal Membrane Oxygenation (ECMO)
This procedure is done if the baby doesn’t respond to other care. With ECMO, blood from the baby’s veins is pumped through an artificial lung. Oxygen is then added and carbon dioxide is removed. The blood is then returned back to the baby. This procedure is only done in certain neonatal intensive care units.
One criterion for the institution of ECMO is an elevated oxygenation index (OI) that is consistently 40 or higher.
Long Term Complications of PPHN
With optimal therapy the mortality rate is now about 10%. Long term complications in survivors of severe PPHN such as neurodevelopmental impairments (e.g. intellectual disabilities, cerebral palsy) and hearing difficulties are about 25%.
References
- Mathew B, Lakshminrusimha S. Persistent pulmonary hypertension in the newborn. Children (Basel). 2017 Jul 28. 4 (8):63. [Medline].
- US food and drug administration. FDA Drug Safety Communication: Selective serotonin reuptake inhibitor (SSRI) antidepressant use during pregnancy and reports of a rare heart and lung condition in newborn babies. Available at http://www.fda.gov/drugs/drugsafety/ucm283375.htm. Accessed: December 14, 2011.
- Steurer MA, Jelliffe-Pawlowski LL, Baer RJ, Partridge JC, Rogers EE, Keller RL. Persistent pulmonary hypertension of the newborn in late preterm and term infants in California. Pediatrics. 2017 Jan. 139 (1):e20161165. [Medline].
- Steurer MA, Baer RJ, Oltman S, et al. Morbidity of persistent pulmonary hypertension of the newborn in the first year of life. J Pediatr. 2019 Aug 6. [Medline].
- Abman SH, Hansmann G, Archer SL, et al. Pediatric pulmonary hypertension: guidelines from the American Heart Association and American Thoracic Society. Circulation. 2015 Nov 24. 132 (21):2037-99. [Medline].
Conclusion
The failure to promptly diagnose and treat babies born with PPHN can tragically result in neurodevelopmental disorders such as intellectual disabilities, cerebral palsy, hearing loss, and death. Neonatal expert witnesses are often called upon in these cases to opine on whether the standard of care has been met.
About the Author
- Usha Raj, MD, MHA is a neonatal perinatal physician and expert witness. She has 35 years’ experience:
- Practiced at UCSF, Harbor-UCLA, and the University of Illinois Chicago
- Director of NICU at Harbor-UCLA for 12 years
- Chief of Neonatology Harbor-UCLA for 13 years
- Director Neonatology Fellowship Training Programs at Harbor-UCLA and UIC
- Published over 192 peer-reviewed manuscripts, reviews and chapters
- Teaches Neonatal Fellows
- Researcher in Pathogenesis of Pulmonary Hypertension with a laboratory continuously funded by National Heart Lung Blood Institute for over 34 years.
- Scientific Recognition, Distinguished Achievement and Elizabeth Rich Awards from the American Thoracic Society
- Julius Comroe Jr. Distinguished Lectureship and election as a fellow by the American Physiological Society
- Honorary doctorate (honoris causa) from the University of Lausanne in recognition of her clinical, scientific and educational achievements
- External Advisor to the Pediatric Pulmonary Hypertension Network of North America.
- Selected for the “U.S.News & World Report” Top Doctors list.